Introduction to Otoplasty
Otoplasty, also known as ear surgery, refers to the surgical procedures for correcting deformities and defects of the pinna (external ear).
The aim and goal of an otoplasty procedure are to produce an external ear with natural proportions, contour and appearance.
The pinna is the only visible part of the ear (the auricle) with its special helical shape. It is the first part of the ear that reacts to sound. The function of the pinna is to act as a kind of funnel that assists in directing the sound further into the ear.
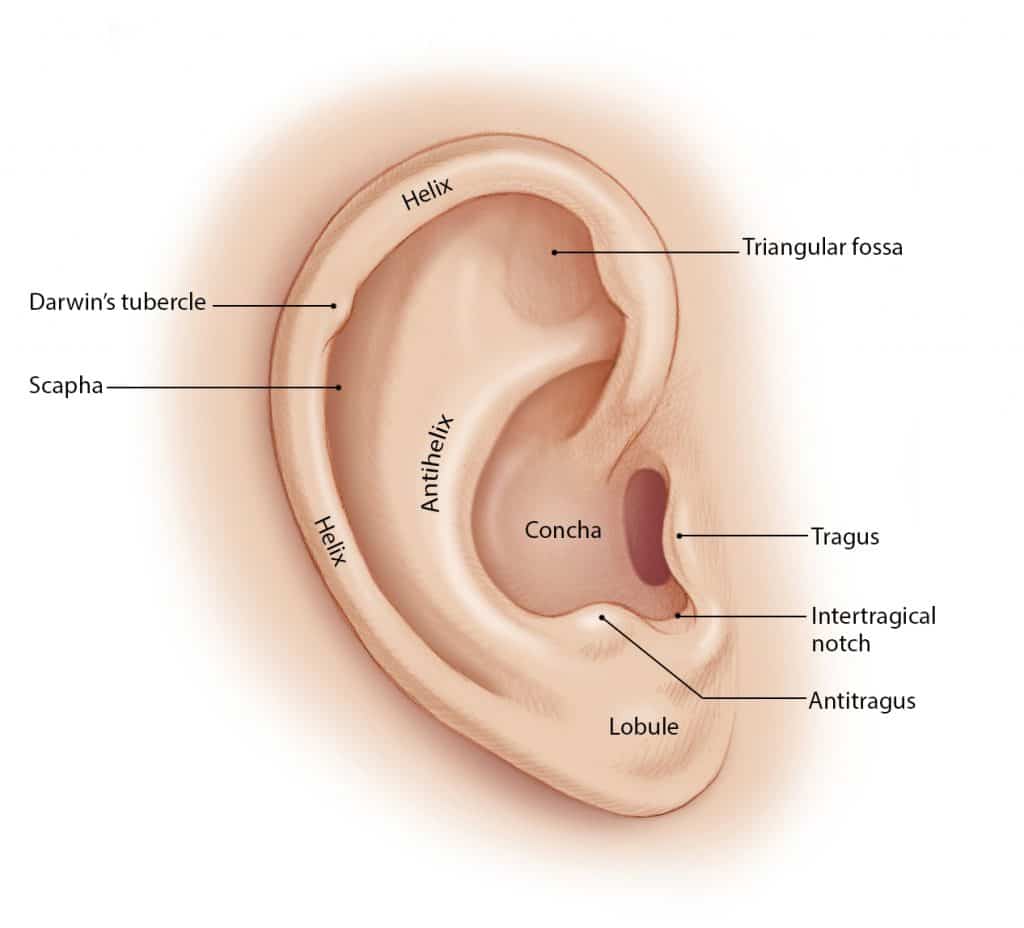
Anatomy Of Ear Pinna (External Ear)
There may be the need for an otoplasty procedure due to birth defects resulting in an underdeveloped pinna (microtia), the complete absence of the pinna (anotia) and trauma to the pinna.
History of Otoplasty
Otoplasty was developed in ancient India by the Ayurvedic physician Sushruta in the 5th century BC. In the 20th and 21st centuries, there have been modern procedures for otoplasty. A pioneer of otoplasty, Dr. Harold Gillies, first reproduced the pinna in 1920.
The development of plastic surgery procedures, such as the refinement of J.F. Dieffenbach’s ear surgery techniques, has established more than 170 otoplasty procedures for correcting prominent ears, and for correcting the defects and deformities of the pinna.
Indications for Otoplasty
Otoplasty is a cosmetic procedure, which means it doesn’t have any profound impact on the function of the ears. It may result in changes in how sound is perceived, but they are almost always subtle that they don’t affect the hearing process.
The surgery is often performed on children six years and above. By this time, the ears have already fully developed and patients are also more likely to be prepared to undergo the procedure.
The indications for the procedure determine the otoplasty techniques that are applied to correct the defect or deformity of the ear. Some of the indications include:
1. Cagot ear – A congenital defect characterized by the absence of an earlobe.
2. Cleft earlobe – A defect characterized by an indentation (notch) to the fleshy portion of the earlobe. The usual correction is the transplantation of an autologous tissue graft.
3. Cryptotia – This is the condition where an ear appears to have its upper portion buried underneath the side of the head.
4. Macrotia – Also known as prominent ears, macrotia refers to an ear that is larger than would be expected.
5. Microtia – A congenital defect characterized by either severe underdevelopment or the absence of the pinna (outer ear).
Types of Otoplasty
There are three main types of otoplasty corrections. They include:
A. Ear augmentation – This addresses the issue of the underdeveloped and absent pinna (microtia and anotia, respectively).
Ear augmentation involves adding structural elements to replace the missing structures. The cartilage tissue grafts for the reconstruction are usually obtained from either ear or the rib cage.
B. Ear pinback – This procedure flattens protruding ears. Ear pinback is usually performed under a local anesthetic with a sedative for adults and general anesthesia for children.
To begin ear pinning surgery, the surgeon makes an incision behind the ear to expose the cartilage.
The cartilage is then reshaped and excess skin is removed. Finally, if necessary, the ear is repositioned more closely to the head, and the incision is closed with non-removable stitches or sutures.
C. Ear reduction – This procedure addresses overdeveloped or prominent ears. Ear reduction might involve reducing one or more of the components of oversized ears; the incisions usually are hidden in, or near, the front folds of the pinna.
Surgical Procedures of Otoplasty
Autoplastic surgery can be performed on a patient under local anesthesia and general anesthesia, usually for children. Cosmetic ear surgery generally lasts between one and two hours, depending on the extent of the surgery.
Depending upon the auricular (pinna) defect, deformity, or reconstruction required, the surgeon applies these three oncoplastic techniques, either individually or in combination, to achieve an outcome that produces an ear of natural proportions, contour, and appearance:
I. Antihelical Fold Manipulation – Following this technique, the surgeon emplaces mattress sutures on the back of the ears, which are tied with sufficient tension to increase the definition of the antihelical fold, thereby setting back the helical rim. The cartilage is not treated.
II. Conchal Alteration – Here, the surgeon decreases the angle (-25 degrees) between the concha and the mastoid process of the head with sutures emplaced between the concha and the mastoid fascia.
II. Correction of Earlobe prominence – Reposition of the earlobe is the most difficult part of otoplasty.
The otoplasty technique most effective for lobular repositioning is the Gosain technique, wherein the surgeon cuts the skin on the medial surface of the earlobe and, when suturing it, takes a bite of the conchal undersurface to pull the earlobe towards the head.
Complications of Otoplasty
Some complications can arise with this procedure include:
- Infection – Cellulitis is rare after otoplasty, but it is treated aggressively with antibiotics to avoid chondritis — which might require debridement and permanently disfigure the ear.
- Hematoma – This is referred to the collection of blood following otoplasty. This otoplasty complication is immediately addressed when the patient complains of excessive pain or when the surgical wound bleeds. The dressing is immediately removed from the ear to ascertain the existence of a hematoma, which is then immediately evacuated.
- Suture complications – The most common otoplasty complication is suture extrusion in the retroauricular sulcus, (the groove behind the ear). Such extruded sutures are easy to remove, but the extrusion occurrence might be associated with granulomas, which are painful and unattractive. This complication might be avoided by using absorbable sutures; to which effect, monofilament sutures are likelier to protrude but have a lesser incidence rate of granulomas; whereas braided sutures are unlikely to protrude but have a greater incidence rate of granulomas.
Recovery
For several days after the surgery, the otoplasty patient wears a voluminous, non-compressive dressing upon the corrected ear(s), during which convalescent period, he or she must avoid excessive bandage pressure upon the ear, lest it causes pain and increases swelling, which might lead to the abrasion (rubbing), or even to the necrosis of the ear’s skin.
After removing the dressing, the patient then wears a loose headband whilst sleeping for a 3–6-week period; it should be snug, not tight because its purpose is to prevent the corrected ear(s) from being pulled forward when the sleeping patient moves whilst asleep.
Hence, a tight headband can abrade and erode the side surface of the ear, possibly creating an open wound. The dressing does not have to be worn if one was operated with the stitch method.
Read More: Rib Removal Surgery


