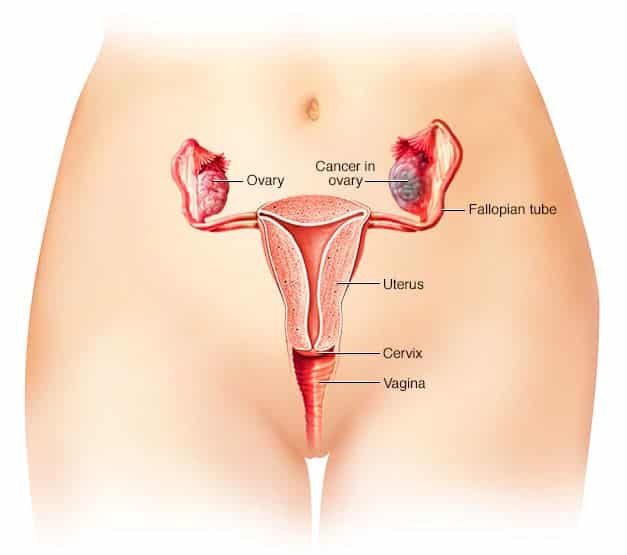
Oophorectomy is the surgical removal of the ovaries. It is often performed to treat diseases such as ovarian cysts, ovarian cancer and to prevent ovarian cancer in high-risk patients. While oophorectomy can be done alone, it is often performed in conjunction with other surgical procedures such as hysterectomy.
Types of Oophorectomy
There are different types of oophorectomy depending on whether a single ovary or both ovaries and other organs are removed.
- Unilateral Oophorectomy – This refers to the removal of one ovary. Here, the woman will still be able to bear children.
- Bilateral Oophorectomy – Removal of both ovaries. The woman will be unable to get pregnant and menopause begins immediately. It is usually done to prevent disorders or the spread of cancer cells.
- Salpingo-oophorectomy – Removal of the fallopian tube along with the ovary.
- Prophylactic oophorectomy – This is also known as elective oophorectomy. The procedure is carried out to reduce the risk of cancer in women with mutation of the BRCA1/2 genes.
Indications for Oophorectomy
Oophorectomy may be medically approved as the best course of action in different situations.
Cancer prevention
Oophorectomy may be indicated in patients with a high risk of developing cancer of the breast and ovaries.
Oophorectomy can significantly improve survival for women with high-risk BRCA mutations, for whom prophylactic oophorectomy around age 40 reduces the risk of ovarian and breast cancer and provides a significant long-term survival advantage. On average, earlier intervention does not provide any additional benefit but increases risks and adverse effects.
Endometriosis
Endometriosis is a disorder in which tissue that normally lines the uterus grows outside the uterus. The main symptoms are pelvic pain and infertility. Oophorectomy may be performed in conjunction with other procedures such as hysterectomy (removal of the uterus) to treat the condition.
Due to its serious side effects, oophorectomy is usually the last resort to treat endometriosis in women of reproductive age.
Ovarian Cysts
Oophorectomy may also be performed to treat ovarian cysts. Some features that may indicate oophorectomy include persistent complex ovarian cysts, ovarian cysts larger than 10 cm, and women who are menopausal or perimenopausal.
Oophorectomy Risks and complications
Although an oophorectomy is often performed to help treat or prevent diseases, it may put women at risk of other issues. The ovaries produce oocytes (eggs) for fertilization and they produce the reproductive hormones, estrogen and progesterone. Its removal means that the woman will be unable to bear a child and also there is a risk of hormonal imbalance.
Surgical risks
The surgery itself also involves some risks, including:
- excessive bleeding or blood clots
- infection
- scar tissue
- nerve damage
- tumor rupture
- injury to the urinary tract or other organs
- hernia due to weakened abdominal muscles
Adverse effect on sexuality
Oophorectomy substantially impairs sexuality. Substantially more women who had both oophorectomy and a hysterectomy reported libido loss, difficulty with sexual arousal, and vaginal dryness than those who had a less invasive procedure.
Cardiovascular risk
Women who undergo oophorectomy have a greater risk of developing a cardiovascular disease such as heart attack, chest pain (angina) or stroke.
Long-term effects
Oophorectomy has serious long-term consequences stemming mostly from the hormonal effects of the surgery and extending well beyond menopause. The reported risks and adverse effects include premature death, cognitive impairment or dementia, parkinsonism, osteoporosis and bone fractures, a decline in psychological well-being, and a decline in sexual function. Hormone replacement therapy does not always reduce the adverse effects.
Oophorectomy Recovery
Women should give themselves plenty of time to recover from surgery, as the recovery time can vary. A woman may want to consider having help at home for the first few days to assist her in getting up and preparing meals.
Women who have had one ovary removed but still have their uterus may notice very little change, as their hormones and menstruation will stay relatively the same. Women who have had both ovaries removed will notice the biggest change.
Doctors can help people to explore recovery options and give them more information about what symptoms to expect after an oophorectomy.
More: Lipoma Removal Cost