Corneal Ulcer Treatment – Overview
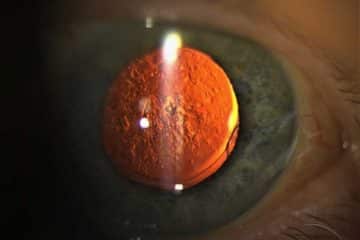
A cornea ulcer, also known as keratitis is an inflammation and subsequent open sore of the cornea.
The cornea overlies the iris, which is the colored part of the eye and is separated from the iris by the aqueous fluid in the anterior chamber of the eye.
It helps in the refraction of light and accounts for about two-thirds of the eye’s total optical power.
Causes of cornea ulcers range from infections from bacteria, fungi, viruses, physical trauma and malnutrition. Cornea ulcer treatment will be based on the cause of the inflammation.
More: What is Blepharospasm all About?
Symptoms of Corneal Ulcer

These include:
- redness of the eye
- severe pain and soreness of the eye
- the feeling of having something in your eye
- tearing
- pus or other discharge
- blurred vision
- sensitivity to light
- swelling of the eyelids
- a white spot on your cornea that you may or may not be able to see when looking in the mirror
See your ophthalmologist immediately if you think you have a corneal ulcer or have any eye symptoms that concern you. Corneal ulcers can badly and permanently damage your vision and even cause blindness if they are not treated.
Causes of Corneal Ulcer
Corneal ulcers are a common human eye disease. They are caused by trauma, particularly with vegetable matter, as well as chemical injury, contact lenses, infections as well as other eye conditions.
Trauma – This refers to damage caused by a direct blow to the eye. Eye trauma often results in cornea ulceration that is centrally located.
Contact Lens – Contact lens wearers particularly are susceptible to eye irritation that can lead to a corneal ulcer. A contact lens may rub against the eye’s surface, creating slight damage to the epithelium that may enable bacteria to penetrate the eye.
Infections – Many micro-organisms cause an infective corneal ulcer. Among them are bacteria, fungi, viruses, protozoa, and chlamydia:
- Bacterial keratitis is caused by Staphylococcus aureus, Streptococcus viridans, Escherichia coli, Enterococci, Pseudomonas, Nocardia, N. Gonorrhoea and many other bacteria.
- Fungal keratitis causes deep and severe corneal ulcers. It is caused by Aspergillus sp., Fusarium sp., Candida sp., as also Rhizopus, Mucor, and other fungi. The typical feature of fungal keratitis is a slow onset and gradual progression, where signs are much more than the symptoms. Small satellite lesions around the ulcer are a common feature of fungal keratitis and hypopyon is usually seen.
- Viral keratitis causes corneal ulceration. It is caused most commonly by Herpes simplex, Herpes zoster and Adenoviruses. Also, it can be caused by coronaviruses & many other viruses. The herpes virus causes a dendritic ulcer, which can recur and relapse over the lifetime of an individual.
- Protozoa infection like Acanthamoeba keratitis is characterized by severe pain and is associated with contact lens users swimming in pools.
- Chlamydia trachomatis can also contribute to the development of a corneal ulcer.
Corneal Ulcer Treatment
Proper diagnosis is essential for optimal treatment. The cause of the ulcer is to be decided. Whether it’s due to an infection or not.
Bacterial corneal ulcers require intensive fortified antibiotic therapy to treat the infection.
Fungal corneal ulcers require the intensive application of topical anti-fungal agents.
Viral corneal ulceration caused by herpes virus may respond to antivirals like topical acyclovir ointment instilled at least five times a day.
Alongside, supportive therapy like pain medications is given, including topical cycloplegics like atropine or homatropine to dilate the pupil and thereby stop spasms of the ciliary muscle.
Superficial ulcers may heal in less than a week. Deep ulcers and descemetoceles may require conjunctival grafts or conjunctival flaps, soft contact lenses, or corneal transplants.
Proper nutrition, including protein intake and Vitamin C, is usually advised in cornea ulcer treatment.
In cases of Keratomalacia, where the corneal ulceration is due to a deficiency of Vitamin A, supplementation of the Vitamin A by the oral or intramuscular route is given.