Spinal Fusion Surgery – Overview
Spinal fusion surgery is an orthopedic procedure that is carried out to join two or more vertebrae. It is also known as spondylodesis and it can be performed at any level in the spine, i.e on the cervical, thoracic or lumbar vertebrae, thereby preventing movement between the fused vertebrae.
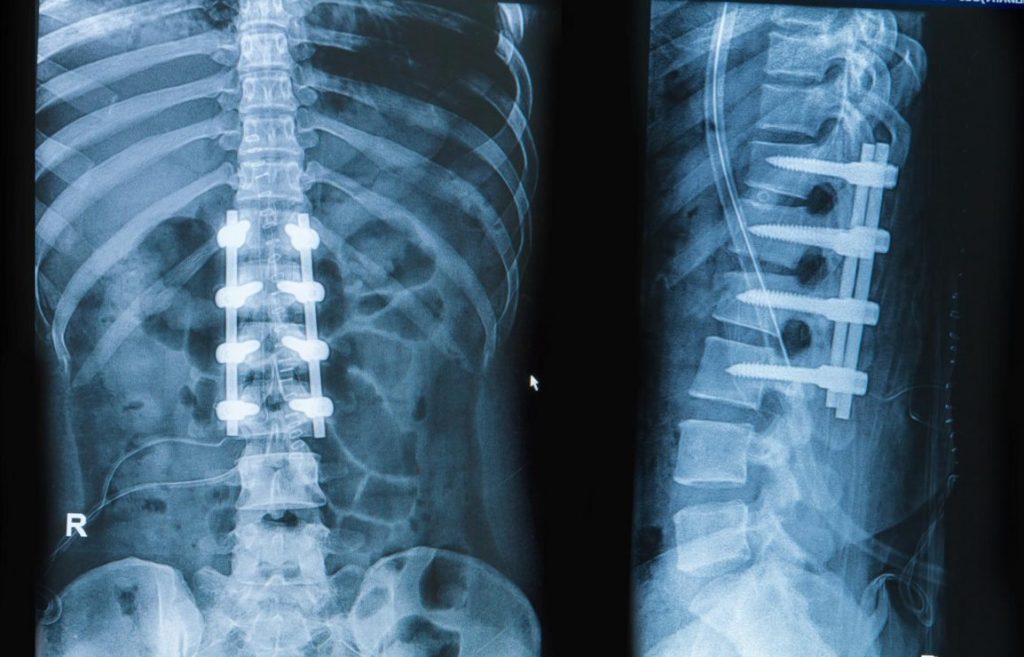
There are many types of spinal fusion surgery depending on the vertebrae and techniques that are involved. Once the vertebra has been fused, bone grafting is done to help the bones heal together and additional hardware (screws, plates, or cages) is often used to hold the bones in place while the graft fuses the two vertebrae.
Spinal fusion surgery is mostly carried out to treat back pain due to degenerative disc diseases, spinal fractures, spinal stenosis, scoliosis, etc.
The Spine
The spine
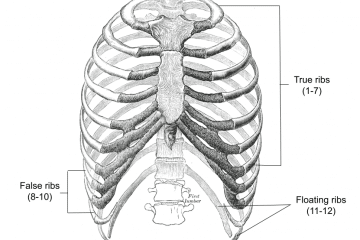
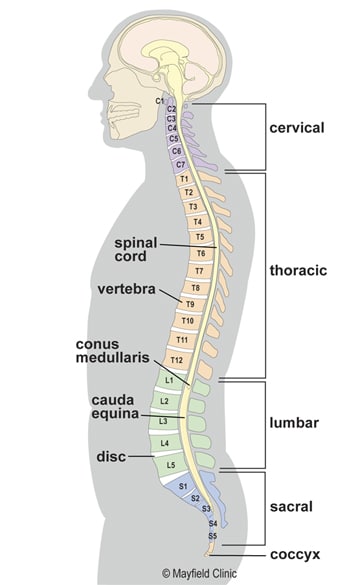
The spine is also known as the vertebral column or backbone is made up of small bones, called vertebrae, which are stacked on top of one another and create the natural curves of your back. It gives you support to stand up straight, and gives you the flexibility to bend and twist. It also protects your spinal cord. The five types of vertebrae bones that make the spine are:
- Cervical vertebrae – The cervical vertebrae of the spine consist of seven bony rings that reside in the neck between the base of the skull and the thoracic vertebrae in the trunk
- Thoracic vertebrae – The thoracic vertebrae are a group of twelve small bones located in the chest region.
- Lumbar vertebrae – The lumbar vertebrae consist of five individual cylindrical bones and they are located in the upper abdomen.
- Sacrum vertebrae – These are located in the lower abdomen
- Caudal vertebrae – These are located in the tail region.
Reasons for Spinal Fusion Surgery
spine fusion surgery
Spinal fusion surgery can be used to treat a variety of conditions affecting any level of the spine—lumbar, cervical and thoracic.
In general, spinal fusion is performed to decompress and stabilize the spine. There are a variety of medical conditions that could cause compression of the spine thereby resulting in back pain and other deformities.
Conditions, where spinal fusion may be considered, include the following:
–Degenerative disc disease: This is an age-related condition that happens when one or more of the discs between the vertebrae of the spinal column deteriorates or breaks down, leading to pain. There may be weakness, numbness, and pain that radiates down the leg.
– Spinal disc herniation: This refers to an injury to the cushioning and connective tissue between vertebrae, usually caused by excessive strain or trauma to the spine.
– Discogenic pain: Discogenic pain is pain originating from a damaged vertebral disc that may be due to a fracture or disease.
– Spinal tumor: This is cancer of the spine and refers to uncontrollable growth of tissues within the spine causing discomfort and pain.
– Scoliosis: Scoliosis is a medical condition in which a person’s spine has a sideways curve. The curve is usually “S”- or “C”-shaped. In some, the degree of curve is stable, while in others, it increases over time. Mild scoliosis does not typically cause problems, while severe cases can interfere with breathing. In that case, a spinal fusion might be needed to straighten the curve as much as possible and stop it from getting worse.
– Vertebral fracture
– Kyphosis
– Spondylolisthesis
– Spondylosis
– Posterior rami syndrome
– Any condition that causes instability of the spine
Spinal Fusion Surgery Procedure
If you have a spinal fusion, you’ll get general anesthesia before the procedure. This lets you sleep through the operation, which takes several hours.
The orthopedic surgeon may follow any of the many types of spinal fusion techniques. Each technique varies depending on the level of the spine and the location of the compressed spinal cord/nerves. After the spine is decompressed, a bone graft or artificial bone substitute is packed between the vertebrae to help them heal together.
In general, fusions are done either on the anterior (stomach), posterior (back), or both sides of the spine.
Today, most fusions are supplemented with hardware (screws, plates, rods) because they have been shown to have higher union rates than non-instrumented fusions.
Minimally invasive techniques are also becoming more popular. These techniques use advanced image guidance systems to insert rods/screws into the spine through smaller incisions, allowing for less muscle damage, blood loss, infections, pain, and length of stay in the hospital.
Related: Types of Hip Surgery
Spinal Fusion Surgery Risks and Complications
As each of the types of surgery, some risks and complications could arise during or after spinal fusion. Complications that could arise during the procedure include:
– Blood loss
– Damage to nerves and surrounding structures.
– Infections: The site of the surgery may become infected with pathogens such as bacteria, viruses, etc. Risk factors include old age, obesity, diabetes, smoking, prior surgery.
– Thrombosis
– Urinary retention
– Deformity: loss of height, alignment, and failure of fusion
– Epidural fibrosis: scarring of the tissue that surrounds the spinal cord
– Death: Spinal fusion is a high-risk surgery and complications can be serious, including death.
Spinal Fusion Surgery Success Rate
Studies indicate that the patient’s pain is improved 60% to 70% after TLIF spinal fusion surgery and approximately 80% of patients undergoing TLIF spinal fusion surgery are satisfied with the surgical result.
Spinal Fusion Surgery Cost
Costs associated with spinal fusion vary depending on the medical institution, insurance, types of surgery, and the overall health of the patient. Total costs typically include labs, medications, room & board, medical supplies, recovery room, operating room services, physical therapy, imaging, and hospital charges. The total cost of the procedure is around $35000 – $75000.
Recovery and What to Expect After Spinal Fusion Surgery
Recovery following spinal fusion is extremely variable, depending on an individual surgeon’s preference and the type of procedure performed. The average length of hospital stay for spinal fusions is 3.7 days. Some patients can go home the same day if they undergo a simple cervical spinal fusion at an outpatient surgery center.
Minimally invasive surgeries are also significantly reducing the amount of time spent in the hospital. Recovery typically involves both restriction of certain activities and rehabilitation training. Restrictions following surgery largely depend on surgeon preference. A typical timeline for common restrictions after a lumbar fusion surgery are listed below:
Walking – most people are out of bed and walking the day after surgery
Sitting – can begin at 1–6 weeks following surgery
Lifting – it is generally recommended to avoid lifting until 12 weeks
Driving – usually can begin at 3–6 weeks
Return to sedentary work – usually between 3–6 weeks
Return to manual work – between 7–12 weeks
Rehabilitation after spinal fusion is not mandatory. There is some evidence that it improves functional status and low back pain so some surgeons may recommend it.
More: Surgical Instruments