Thyroidectomy – Overview
A goiter, or goitre, is a swelling in the neck resulting from an enlarged thyroid gland. A goiter can be associated with a thyroid that is not functioning properly.
Generally, over 90% of goiter cases are due to iodine deficiency.
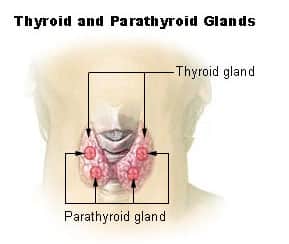
The thyroid gland produces two main hormones — thyroxine (T-4) and triiodothyronine (T-3). These hormones circulate in the bloodstream and help regulate metabolism.
They maintain the rate at which the body uses fats and carbohydrates, help control the body temperature, influence the heart rate, and help regulate the production of proteins.
The thyroid gland also produces calcitonin — a hormone that helps regulate the amount of calcium in your blood.
Depending on the cause, if the thyroid gland is producing excess amounts of hormones; radioactive iodine is given to the patient to shrink the gland.
Otherwise, if goitre is caused by iodine deficiency, small doses of iodide in the form of Lugol’s iodine or KI solution are given. In some cases, thyroidectomy may be performed to treat goiter. Thyroidectomy is a surgery performed to remove all or part of the thyroid gland.
Thyroidectomy Procedure
A thyroidectomy is a surgical procedure to remove all or part of the thyroid gland and is used to treat diseases of the thyroid gland including:
- Thyroid cancer
- Hyperthyroidism (overactive thyroid gland)
- Large goiters or thyroid nodules causing symptomatic obstruction such as swallowing or breathing difficulties.
- Multi-nodular Goiter
- A thyroidectomy is traditionally a minimally invasive surgery performed through a small horizontal incision in the front of the neck. The entire thyroid gland may be removed or just a single lobe, a portion of a lobe and the isthmus or other structures. Depending on the extent of the operation, patients may need to take the drug levothyroxine, an oral synthetic thyroid hormone.
Types of Thyroidectomy
There are different types of thyroidectomy depending on the extent to which the thyroid gland is removed. These include:
Hemithyroidectomy—Entire isthmus is removed along with 1 lobe. Done in benign diseases of only 1 lobe.
Subtotal thyroidectomy—Removal of the majority of both lobes leaving behind 4-5 grams (equivalent to the size of a normal thyroid gland) of thyroid tissue on one or both sides—this used to be the most common operation for multinodular goiter.
Partial thyroidectomy—Removal of gland in front of the trachea after mobilization. Done in nontoxic MNG. Its role is controversial.
Near-total thyroidectomy—Both lobes are removed except for a small amount of thyroid tissue (on one or both sides) in the vicinity of the recurrent laryngeal nerve entry point and the superior parathyroid gland.
Total thyroidectomy—Entire gland is removed. Done in cases of papillary or follicular carcinoma of the thyroid, medullary carcinoma of the thyroid. This is now also the most common operation for multinodular goitre.
Risks and complications of Thyroidectomy
As with every surgical operation, there are risks of complications involved with thyroidectomy. They include:
- Bleeding – There is a risk of excessive bleeding due to the surgery.
- Infection – At about a 2% rate. Drainage is an important part of treatment. Possibly an increased risk with chronic pre-operative steroid use.
- Hypothyroidism – This refer to a condition in which your thyroid gland doesn’t produce enough of certain crucial hormones. This is to be expected as the thyroid glands have been removed and it occur in up to 50% of patients after ten years. After the removal of thyroid, patients usually take a prescribed oral synthetic thyroid hormone—levothyroxine (Synthroid)—to prevent hypothyroidism.
Thyroidectomy Cost
The total cost for thyroid surgery depends on a lot of factors such as the anesthetic fee, private hospital fee, private operating facility fee, the extent of surgery required.
The total cost of the procedure is around $5500 – $7500.


