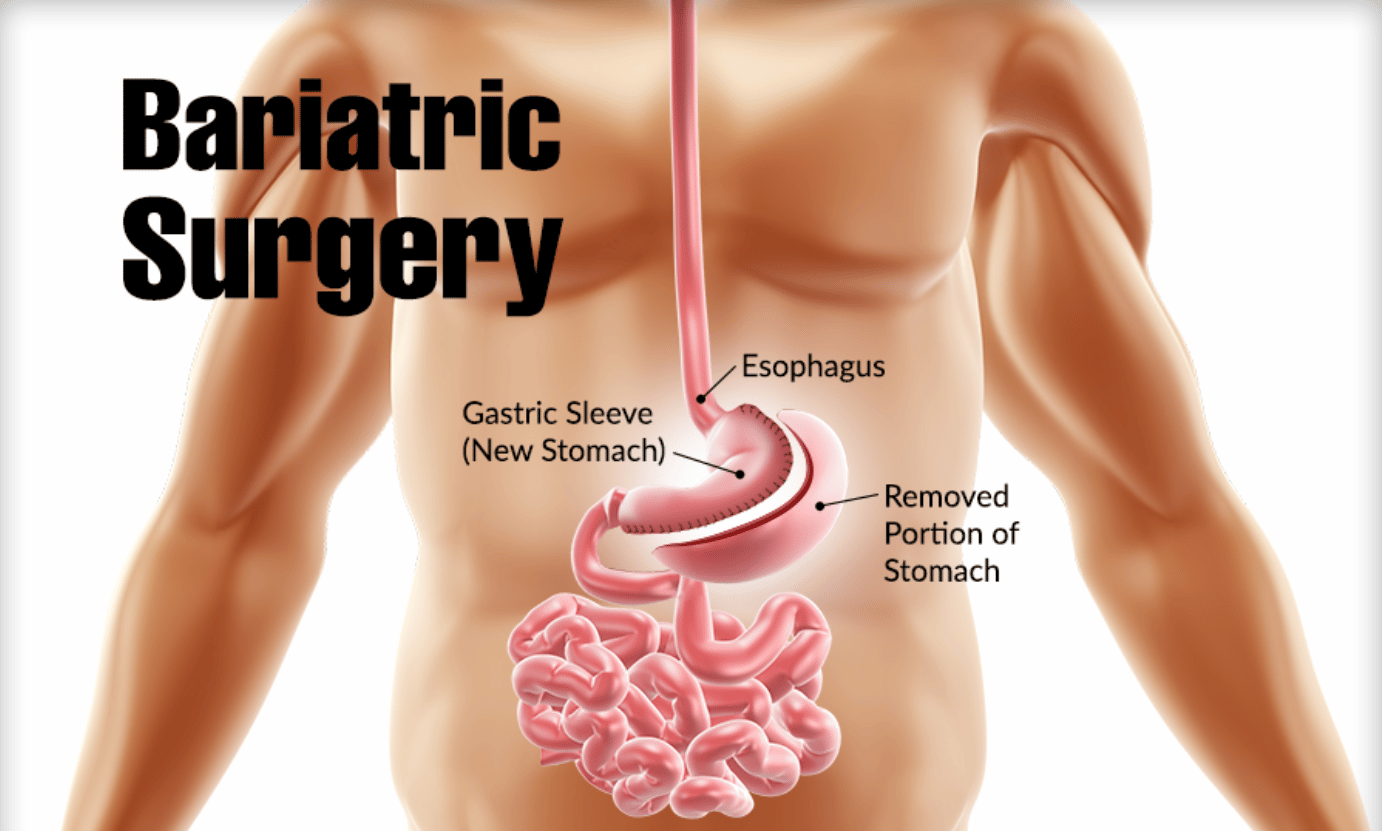
Bariatric Surgery
Bariatric surgery, also known as weight loss surgery and obesity surgery, includes a variety of surgical procedures performed on people who have obesity.
Bariatric surgical procedures cause weight loss by restricting the amount of food the stomach can hold, causing malabsorption of nutrients, or by a combination of both gastric restriction and malabsorption.
Bariatric Surgery
Studies have shown that bariatric surgery causes significant long-term weight loss, recovery from diabetes and improvement in cardiovascular risk factors.
It is recommended for obese people with a body mass index (BMI) of 40 and above and for people with a BMI of 35 to 40 and serious coexisting medical conditions such as diabetes.
Medical Uses of Bariatric Surgery
Bariatric surgery is very important for procedures for people with morbid obesity who have failed with an exercise plan. The medical uses of the procedure include:
Weight Loss
According to American College Physicians, bariatric surgery should be considered as a treatment option for people with severe obesity. Such people must have tried exercise and diet programs but failed.
The U.S National Institute of Health recognized bariatric surgery as the only effective treatment to combat severe obesity and maintain weight loss in the long term. Weight loss leads to an improvement of the overall health and other benefits such as the decreased risk of diabetes, decreased risk of heart disease, decreased joint pain, decreased risk of stroke and lowered blood pressure.
Psychological Health
Some studies have shown that psychological health can improve following bariatric surgery.
Types of Bariatric Surgery
Procedures can be grouped into three main categories namely:
- Blocking Procedures
- Restricting Procedures
- Mixed Procedures
1. Blocking Procedures
These types of procedures block the absorption of food leading to malabsorption. Generally, these blocking procedures lead to more weight loss than the restrictive procedures but they are riskier.
a. Biliopancreatic diversion
The original version of this procedure has been stopped due to problems with it. It has been modified with the inclusion of a duodenal switch (DS). So it’s also known as biliopancreatic diversion with duodenal switch (BPD/DS).
Part of the stomach is resected, creating a smaller stomach and then the distal part of the small intestine is connected to the pouch. The duodenum and jejunum parts of the small intestine are essentially bypassed.
The malabsorptive effect of BPD/DS is so potent and that the patients who undergo the procedure must take vitamin supplements for life. In around 2% of patients, there is severe malabsorption and nutritional deficiency that requires restoration of normal absorption.
Advantages
– BPD/DS results in greater weight loss compared to other procedures.
– It is more effective against diabetes.
– It is fully reversible as no part of the small intestine is removed.
Disadvantages
– Has a greater potential to cause protein deficiencies and long-term deficiencies in several vitamins and minerals, i.e. iron, calcium, zinc, fat-soluble vitamins such as vitamin D
– There is a need for long-term nutritional follow-up and monitoring of BPD/DS patients.
– BPD/DS patients have a higher occurrence of smelly flatus and diarrhea
b. Jejunoileal bypass
This procedure is no longer performed. It was a surgical weight-loss procedure performed for the relief of morbid obesity from the 1950s through the 1970s in which all but 30 cm (12 in) to 45 cm (18 in) of the small bowel was detached and set to the side.
2. Restricting Procedures
Rather than block out the absorption of nutrients, restricting bariatric procedures shrink the size of the stomach making people feel fuller when they eat less.
a. Sleeve gastrectomy
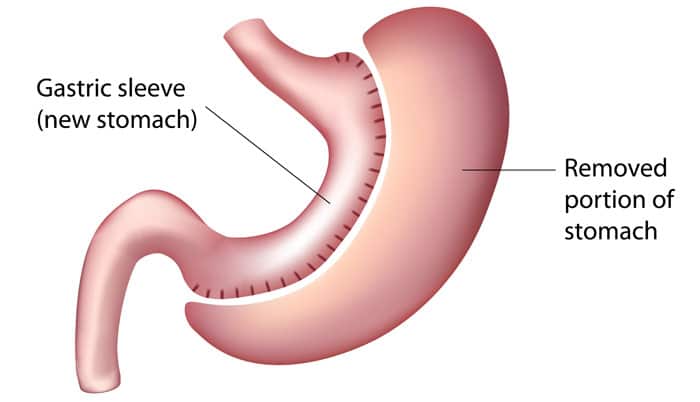
Sleeve gastrectomy is a surgical weight-loss procedure in which the stomach is reduced to about 15% of its original size, by surgical removal of a large portion of the stomach along the greater curvature. The result is a sleeve or tube-like structure. The procedure permanently reduces the size of the stomach, although there could be some dilatation of the stomach later on in life. The procedure is generally performed using minimally invasive techniques and is irreversible.
b. Stomach folding
This procedure is similar to the gastric sleeve but there is no removal of stomach tissue and the sleeve is created by suturing parts of the stomach. The natural nutrient absorption capabilities of the stomach are also preserved.
c. Vertical banded gastroplasty
In the vertical banded gastroplasty, also called the Mason procedure or stomach stapling, a part of the stomach is permanently stapled to create a smaller pre-stomach pouch, which serves as the new stomach.
d. Adjustable gastric band

The restriction of the stomach also can be created using a silicone band, which can be adjusted by the addition or removal of saline through a port placed just under the skin. This operation can be performed laparoscopically, and is commonly referred to as a “lap band”.
Weight loss is predominantly due to the restriction of nutrient intake that is created by the small gastric pouch and the narrow outlet. [31] It is considered one of the safest procedures performed today with a mortality rate of 0.05%.
e. Intragastric balloon
Gastric Balloon
This procedure involves the placement of a deflated gastric balloon into the stomach and then filling it to decrease the amount of gastric space.
A gastric balloon, also known as a stomach balloon, is an inflatable medical device that is temporarily placed into the stomach to reduce weight. It is marketed to provide weight loss when diet and exercise have failed and surgery is not wanted or not recommended.
The balloon is placed in the stomach at most for 6 months during which period there is an average weight loss of 5-9 BMI.
3. Mixed Procedures
These procedures apply both blocks and restrict at the same time.
a. Gastric Bypass Surgery
![]()
This refers to a surgical procedure in which the stomach is divided into a small upper pouch and a much larger lower pouch and then the small intestine is rearranged to connect to both. Surgeons have developed several ways to reconnect to the intestine leading to several types of gastric bypass procedures.
Following the GBP procedure, there is a marked reduction in the functional volume of the stomach and a change in the physiological response to food. The patient feels full after consuming a less diet.
b. Implantable gastric stimulation
This procedure where a device similar to a heart pacemaker is implanted by a surgeon, with the electrical leads stimulating the external surface of the stomach, is being studied in the USA.
Electrical stimulation is thought to modify the activity of the enteric nervous system of the stomach, which is interpreted by the brain to give a sense of satiety, or fullness. Early evidence suggests that it is less effective than other forms of bariatric surgery.
Bariatric Surgery Risks, Complications, and Side Effects
All surgical procedures carry risks. Some bariatric surgery risks include:
- Acid reflux
- Anesthesia-related risks
- Chronic nausea and vomiting
- Dilation of esophagus
- Inability to eat certain foods
- Infection
- Obstruction of stomach
- Weight gain or failure to lose weight
Bariatric surgery carries some long-term risks for patients, including:
- Dumping syndrome is a condition that can lead to symptoms like nausea and dizziness
- Low blood sugar
- Malnutrition
- Vomiting
- Ulcers
- Bowel obstruction
- Hernias
Bariatric Surgery Recovery
Immediately after bariatric surgery, the patient is restricted to a clear liquid diet such as clear broth, diluted fruit juices or sugar-free drinks.
This diet is continued until the gastrointestinal tract has recovered from the surgery. Food high in carbohydrates is best avoided during the initial weight-loss period.
Post-surgery, overeating is curbed because exceeding the capacity of the stomach causes nausea and vomiting. Diet restrictions after recovery from surgery depend in part on the type of surgery.
Many patients will need to take a daily multivitamin pill for life to compensate for reduced absorption of essential nutrients. Because patients cannot eat a large quantity of food, physicians typically recommend a diet that is relatively high in protein and low in fats and alcohol.
More: Stomach Ulcer Surgery